Surgical
Autonomy
Program
A platform to assess competency,
provide feedback and visualize progress
for surgical trainees in the OR setting.
Surgical
Autonomy
Program
A platform to assess competency,
provide feedback and visualize
progress for surgical trainees in
the OR setting.
Surgical Autonomy Program
A platform to assess competency, provide feedback and visualize progress for surgical trainees in the OR setting.
Surgical Autonomy Program Overview
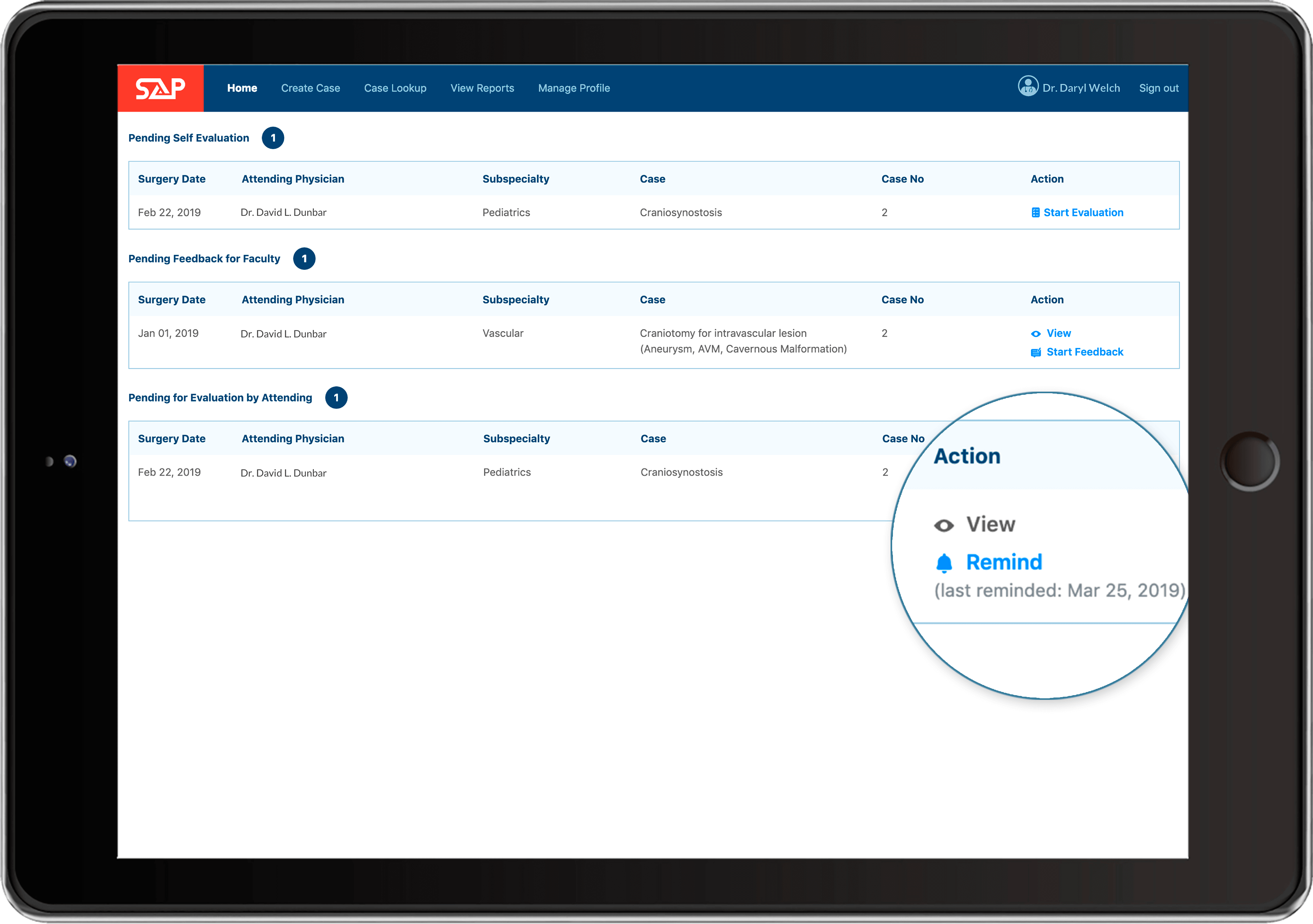
Simple and Flexible
About Surgical Autonomy Program
"Residency Programs need a better way to provide autonomy, feedback and improve meta cognitive skills."The program has been developed at Duke University’s Department of Neurosurgery to address what it means to “educate” and “assess competence” in the environment, shaped by a number of factors: decreased junior resident case volumes due to the ACGME work-hour regulations, pressure to increase operative volume (RVUs), and challenges such as the “teaching” being inherently inefficient and a poor understanding on the part of a vast number of faculty as to how learners learn (how to teach).
Surgical Residency Training is essentially an apprenticeship; hence, Surgical Autonomy Program took the approach of applying Vygotsky’s Social Learning Theory to the process of one’s acquisition of surgical skills. The Social Learning Theory states that the metacognitive skills where pre-existing knowledge of the MKO–More Knowledgeable Other (faculty) leads the learner (resident) through the ZPD– Zones of Proximal Development chosen by the learner where the learner is most motivated to learn, agreed upon by the MKO.
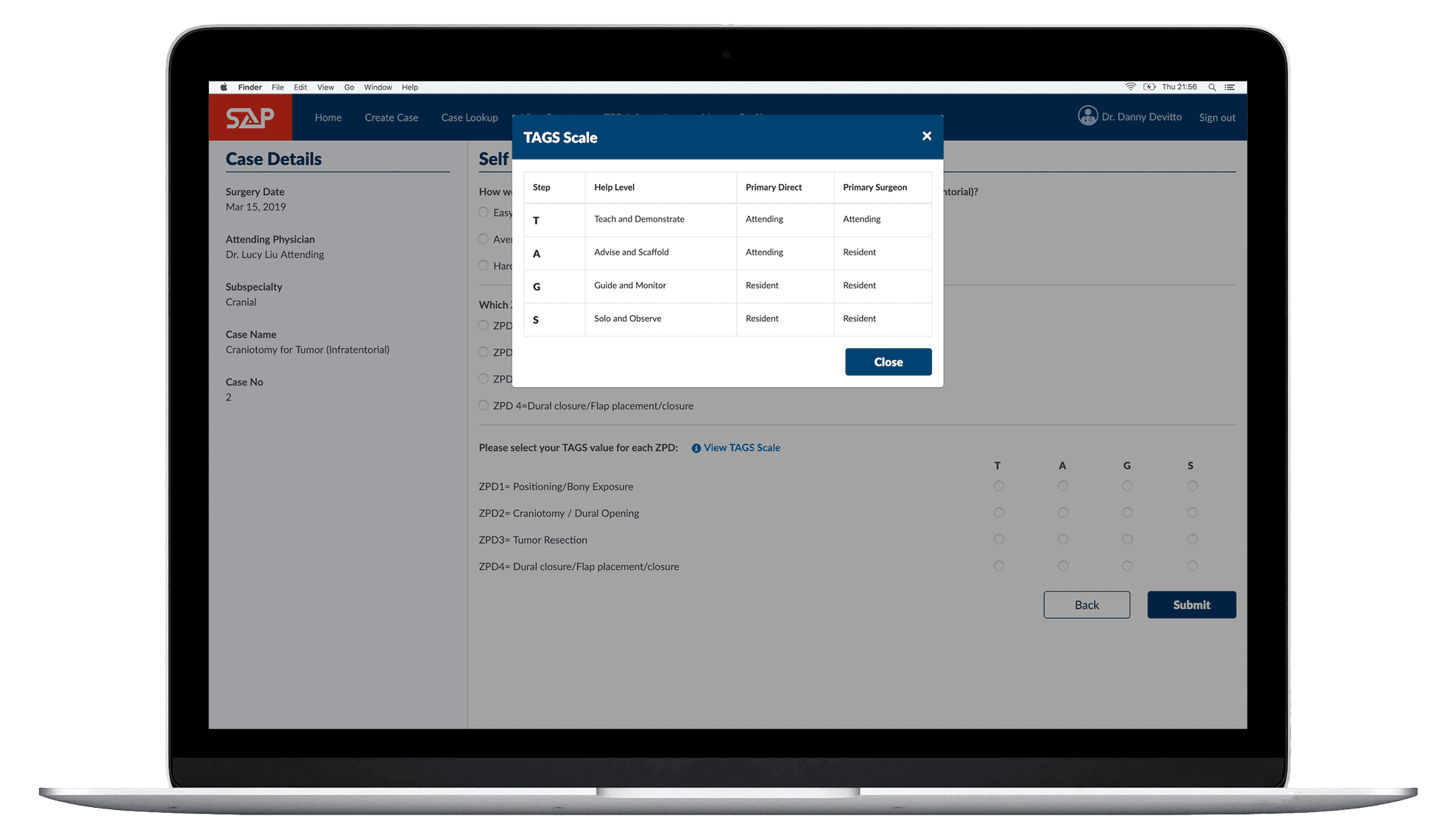
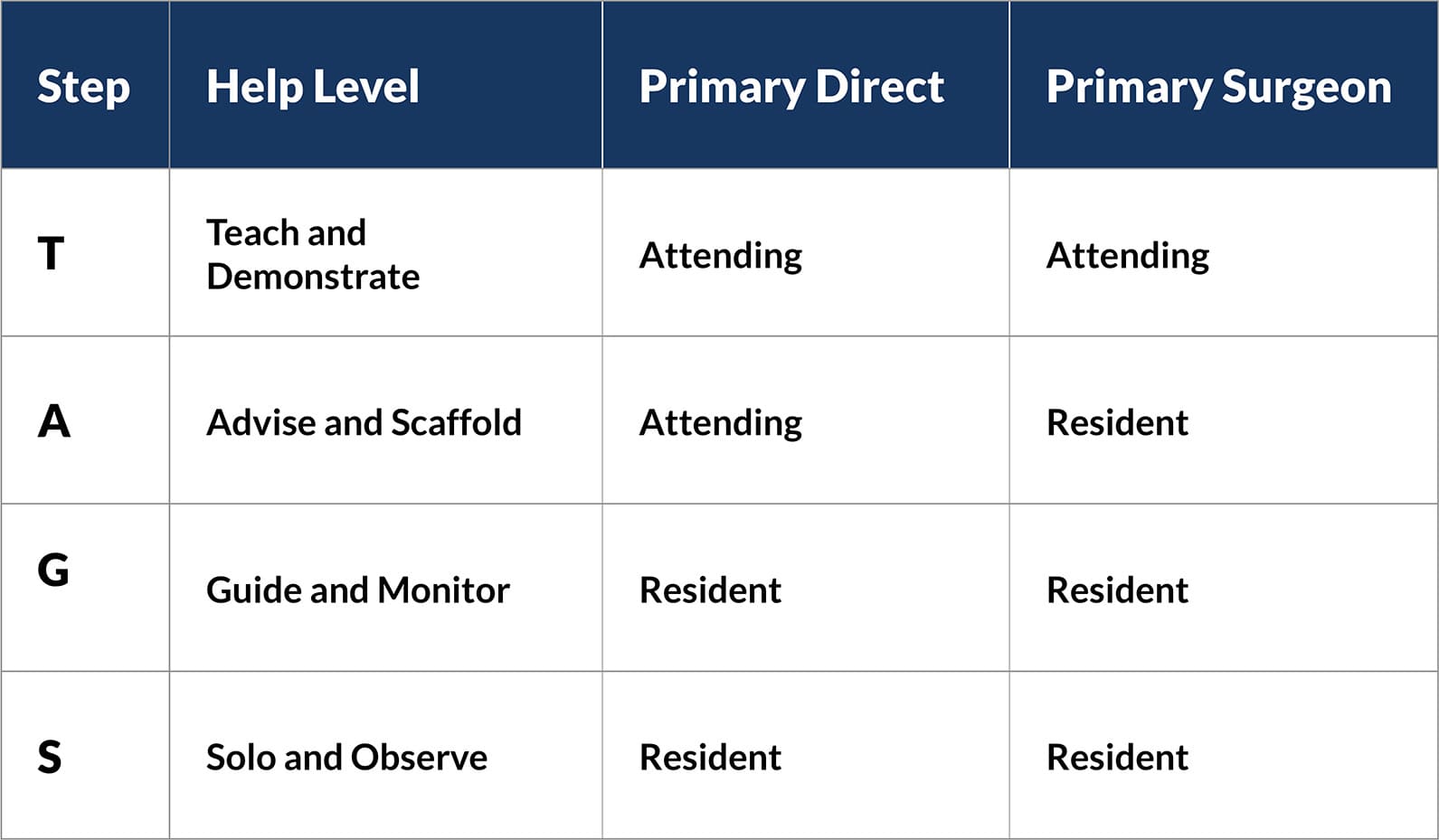
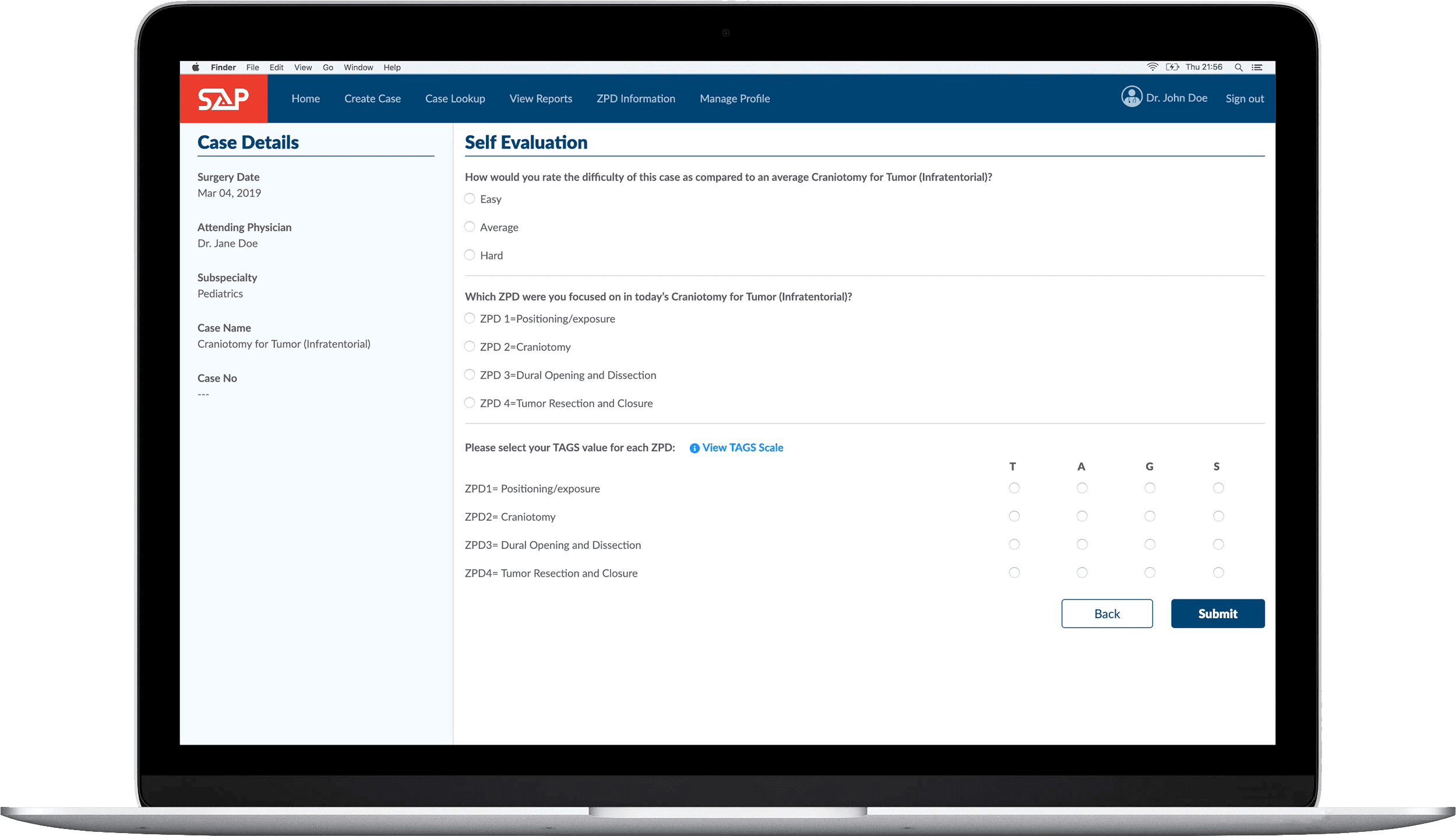
Proper instruction and scaffolding in the Zones of Proximal Development leads to integration of factual and cognitive knowledge as well as psychomotor skills. In keeping with this, the Surgical Autonomy Program approach divides each surgical procedure into four Zones of Proximal Development (ZPD). A resident’s progress is assessed along each ZPD, using a simple scale called TAGS™. Surgical Autonomy Program further encourages formative (versus summative) feedback from the MKO to the learner.
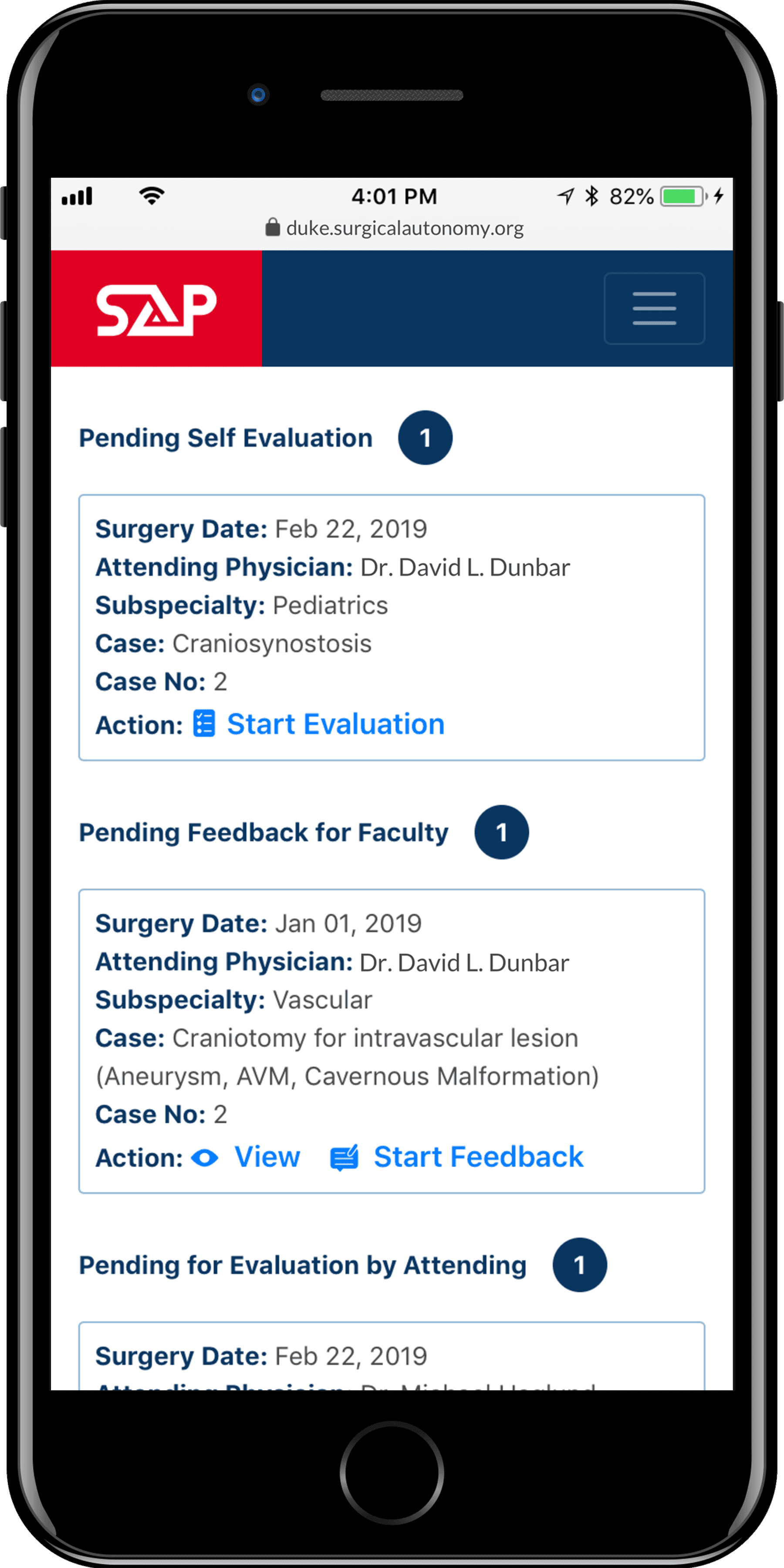
 The evaluations take
The evaluations take less than a minute to complete
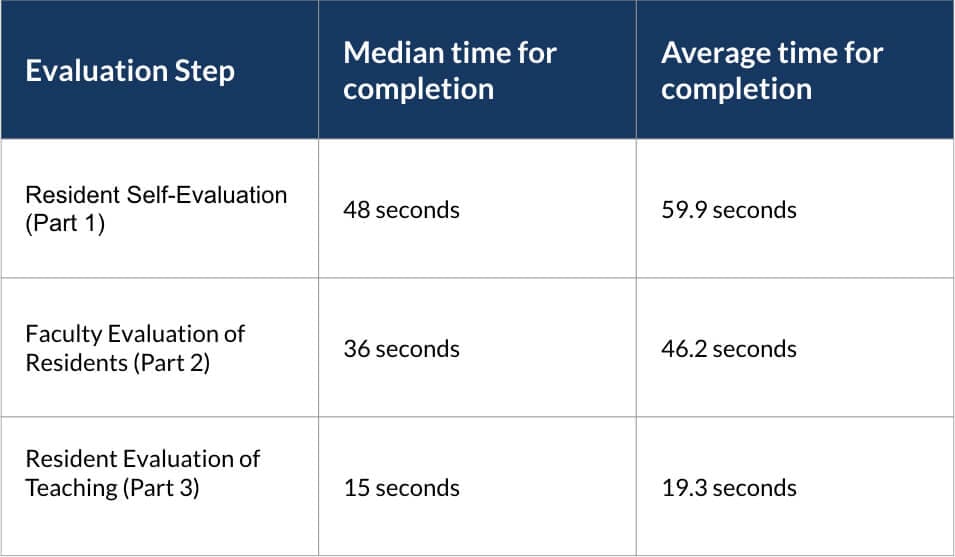 (Times computed from the pilot at Duke Neurosurgery using 1279 case evaluations)
(Times computed from the pilot at Duke Neurosurgery using 1279 case evaluations)
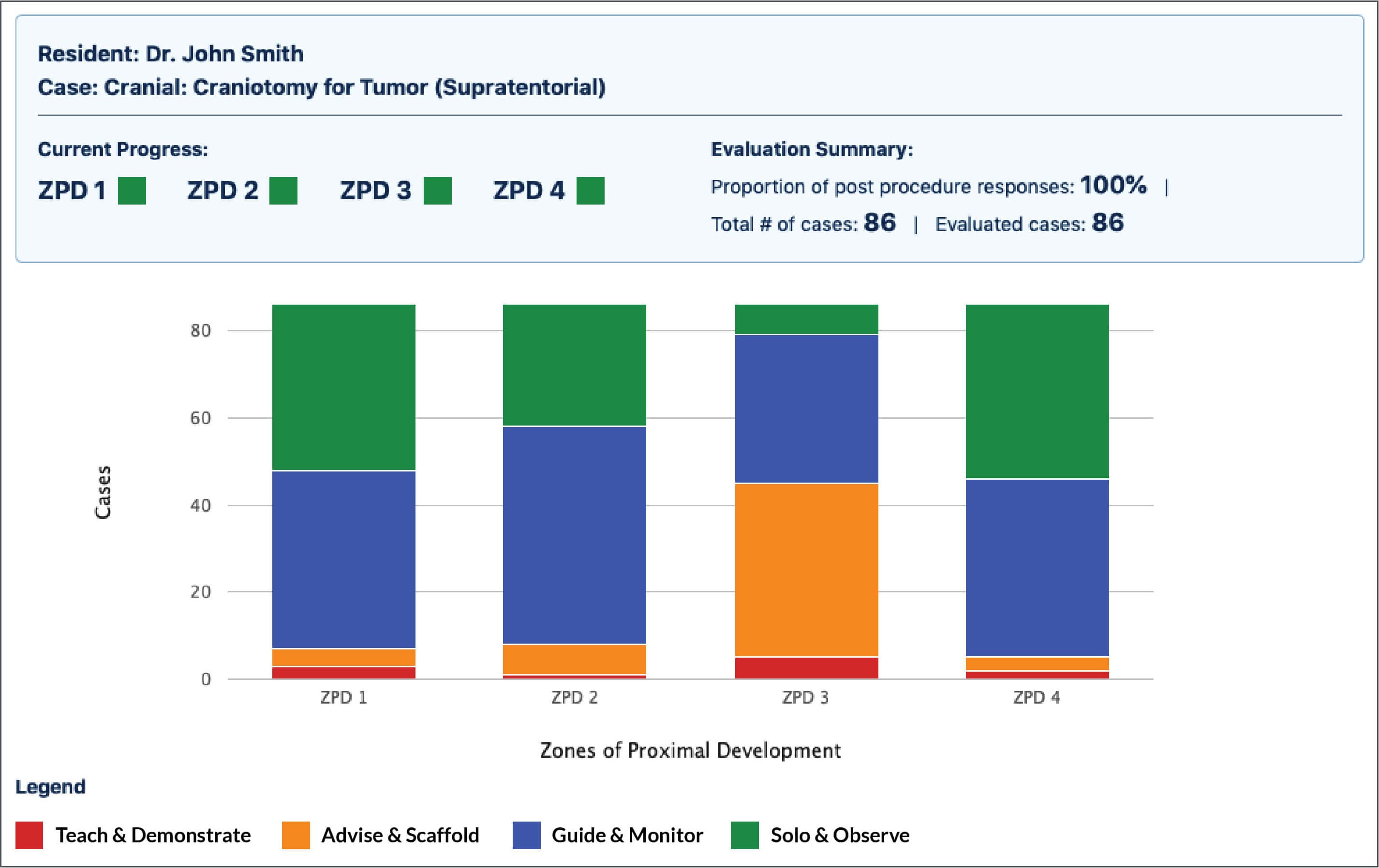
 Easily and clearly visualize Resident
Easily and clearly visualize Resident progress through ZPD
Salient Features
TAGS™ Scale